Helicobacter Pylori
This unusual name identifies the bacteria that can cause infection in the stomach. Bacteria are tiny microbes, larger than viruses, but still only seen under the microscope. To understand how and where the infection occurs, it is useful to know the anatomy of the upper digestive tract. The food pipe is called the esophagus. It enters into the upper part of the stomach, where food collects. The narrower, lower part of the stomach is called the antrum. The antrum contracts frequently and vigorously, grinding up the food and squirting it into the small intestine. The stomach, including the antrum, is covered by a layer of mucous, which protects it from the strong acid that the stomach secretes.
The Infection
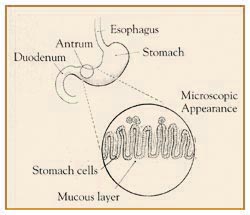 Helicobacter pylori is a fragile bacteria that has found an ideal home in the protective mucous layer of the antrum of the stomach. It has several long protruding threads that attach themselves to the side of the underlying stomach cells. The germ is protected in this mucous environment. It does not infect the stomach cells as certain other bacteria might. The infection, however, does generate a reaction in the body. Infection-fighting white blood cells move into the area and the body even develops protein antibodies to the bacteria, so the infection is indeed very real. It is still uncertain how this infection occurs. It is probably acquired by ingesting contaminated food or cooking with contaminated utensils. Older people have a higher incidence of the infection, as do people in Third World countries where contaminated foods are more frequently found. The infection, however, remains localized and can persist indefinitely unless specific treatment is given.
Helicobacter pylori is a fragile bacteria that has found an ideal home in the protective mucous layer of the antrum of the stomach. It has several long protruding threads that attach themselves to the side of the underlying stomach cells. The germ is protected in this mucous environment. It does not infect the stomach cells as certain other bacteria might. The infection, however, does generate a reaction in the body. Infection-fighting white blood cells move into the area and the body even develops protein antibodies to the bacteria, so the infection is indeed very real. It is still uncertain how this infection occurs. It is probably acquired by ingesting contaminated food or cooking with contaminated utensils. Older people have a higher incidence of the infection, as do people in Third World countries where contaminated foods are more frequently found. The infection, however, remains localized and can persist indefinitely unless specific treatment is given.
Gastritis
Inflammation of the stomach is called gastritis. Gastritis can be caused by consuming excessive alcohol and by certain drugs, such as aspirin and arthritis drugs like ibuprofen. Helicobacter pylori bacteria can also cause gastritis. The infection has been found in every part of the world, in every part of society, and in every age group. The infection tends to be more common where sanitation is less effective, so it occurs more quickly in younger people in Third World countries. However, the infection does increase with age everywhere, indicating its wide prevalence. In fact, this infection is probably one of the most common infections in the world. In many, perhaps most cases, it does not produce symptoms. In other words, the infection can occur without the individual knowing it. Infection, at times, can lead to an ulcer. The symptoms of gastritis are upper abdominal burning, bloating, and discomfort. Nausea and even vomiting may also occur.
Non-Ulcerative Dyspepsia
At times, a person may have symptoms that suggest ulcers. These include burning or pain in the upper abdomen, often occurring an hour or so after meals or even during the night. These symptoms are often temporarily relieved by antacids, milk, or medications that reduce stomach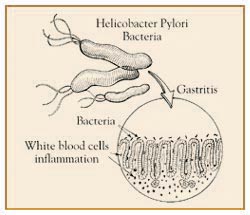 acidity. Yet, the physician does not find an ulcer when the patient is tested by x-ray or endoscopy (a visual scope exam of the stomach). If helicobacter pylori is found in the stomach, it is tempting to believe that it is the cause of the symptoms. At times, a physician will use antibiotic therapy to see if clearing the infection relieves symptoms.
acidity. Yet, the physician does not find an ulcer when the patient is tested by x-ray or endoscopy (a visual scope exam of the stomach). If helicobacter pylori is found in the stomach, it is tempting to believe that it is the cause of the symptoms. At times, a physician will use antibiotic therapy to see if clearing the infection relieves symptoms.
Duodenal Ulcers
The duodenum is the first portion of the intestine beyond the stomach. In times past, physicians were taught "no acid, no ulcer." This statement means that the medical profession felt the single most important factor in duodenal ulcer formation was strong stomach acid. Research has now demonstrated that almost all patients who develop duodenal ulcers have helicobacter pylori infection in the stomach as well. Medical studies are under way to determine the relationship between the two, and how an infection in the stomach can be related to a duodenal ulcer. Acid is still important. So is aspirin and arthritis medication like ibuprofen. Increasingly, however, physicians are accepting the fact that the infection is related somehow to the development of duodenal ulcers. It is now rather easy to clear duodenal ulcers with the strong acid reducing medicines available. But ulcers usually recur unless the Helicobacter pylori infection is cleared.
Stomach Ulcers
Ulcers can develop in the stomach as well, and in these instances, the Helicobacter pylori infection is found in 60 to 80 percent of cases. Again, it is still uncertain how the infection acts to cause the ulcer. It probably weakens the protective mucous layer of the stomach. This allows acid to seep in and injure the underlying stomach cells. There is still a good deal of research that needs to be done to unravel this relationship, however.
The Diagnosis
There are several ways to make the diagnosis. During endoscopy, the physician may remove small samples of tissue for testing. A simple breath test, when available, can diagnose the infection. In this test, a substance called urea is given by mouth. A strong enzyme in the bacteria breaks down the urea into an ammonia gas which is then exhaled through the lungs and can he measured. And finally, there is a blood test that measures the protein antibodies in the blood against the bacteria.
When Is Treatment Necessary?
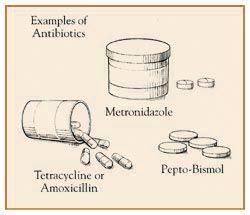 Since the infection is so common and often does not cause symptoms, it is presently recommended that no treatment be given under these circumstances. If ulcers have occurred in the stomach or duodenum, treatment with antibiotics is strongly recommended. It must be remembered that the microbe is buried deep in the stomach mucous, so it is difficult to get rid of this infection. Therefore, several antibiotics are generally used together to prevent the germ from developing resistance to any one of them. Current medical studies are being done to develop easier treatment programs for this difficult infection.
Since the infection is so common and often does not cause symptoms, it is presently recommended that no treatment be given under these circumstances. If ulcers have occurred in the stomach or duodenum, treatment with antibiotics is strongly recommended. It must be remembered that the microbe is buried deep in the stomach mucous, so it is difficult to get rid of this infection. Therefore, several antibiotics are generally used together to prevent the germ from developing resistance to any one of them. Current medical studies are being done to develop easier treatment programs for this difficult infection.
In Summary…
Helicobacter pylori is a very common infection of the stomach. In most cases, it causes no problems or symptoms. It is now clear that the infection is related to the development of stomach and duodenal ulcers. However, stomach acid is still a factor in the development of most ulcers. Increasingly, physicians are treating the underlying infection with antibiotics. The physician is able to evaluate this infection and arrive at the appropriate recommendation and treatment program.
Hiatal Hernia
The hiatal hernia is one of the most misunderstood and maligned conditions in medicine. People blame this hernia for much more than it ever does. Patients with a hiatal hernia need to understand what it is and what might occur with it. Most importantly, they need to know it is unusual for serious problems to develop from this type of hernia.
 Anatomy
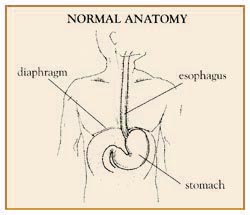
Anatomy
The diaphragm is a sheet of muscle that separates the lungs from the abdomen. When a person takes a deep breath, the dome-shaped diaphragm contracts and flattens. In doing this, the diaphragm pulls air into the lungs. The left diaphragm contains a small hole through which passes the tube-shaped esophagus that carries food and liquid to the stomach. Normally this hole, called a hiatal, is small and fits snugly around the esophagus. The J-shaped stomach sits below the diaphragm.
What Causes a Hiatal Hernia?
In some people, the hiatal or hole in the diaphragm weakens and enlarges. It is not known why this occurs. It may be due to heredity, while in others it may be caused by obesity, exercises such as weightlifting, or straining at stool. Whatever the cause, a portion of the stomach herniated, or moves up, into the chest cavity through this enlarged hole. A hiatal hernia is now present. Hiatal hernias are very common, occurring in up to 60 percent of people by age 60.
What Are the Different Types of Hiatal Hernia?
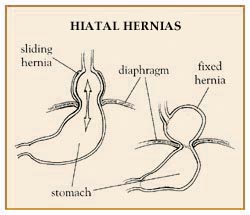
- Sliding Hiatal Hernia-In this most common type of hiatal hernia, the herniated portion of thestomach slides back and forth, into and out of the chest. These hernias are normally small and usually cause no problems or even symptoms.
- Fixed Hiatal Hernia-In this case, the upper part of the stomach is caught up in the chest. Even with this hernia, there may be few symptoms. However, the potential for problems in the esophagus is increased.
- Complicated or Serious Hiatal Hernia--Fortunately, this type of hernia is uncommon. It includes a variety of patterns of herniation of the stomach, including cases in which the entire stomach moves up in the chest. There is a high likelihood that medical problems will occur with this hernia and that treatment, frequently involving surgery, will be required. Complicated hernias are uncommon.
Symptoms
In most patients, hiatal hernias cause no symptoms. This is especially true of sliding hernias. When symptoms occur, they may only be heartburn and regurgitation, when stomach acid refluxes back into the esophagus. Some patients with fixed hiatal hernias experience chronic reflux of acid into the esophagus, which may cause injury and bleeding. Anemia, or low red blood cell count can result. Further, chronic inflammation of the lower esophagus may produce scarring and narrowing in this area. This, in turn, makes swallowing difficult, and food does not pass easily into the stomach.
Does Hiatal Hernia Cause Pain and Indigestion?
It is wrong to always blame a hiatal hernia for pain and indigestion. Hiatal hernias generally do not cause acute pain. This symptom may result from other disorders, such as peptic ulcers or even heart disease. Some patients with coronary heart disease fool themselves into believing their discomfort is due to a hiatal hernia. If upper abdominal pain or indigestion occurs, people should not mislead themselves into thinking the cause is a hiatal hernia. Instead, the patient should seek medical advice.
Diagnosis
Diagnosis of a hiatal hernia is typically made through an upper GI barium x-ray. A complementary test is gastroscopy, or upper intestinal endoscopy, in which the physician visually examines the esophagus and stomach using a flexible scope while the patient is lightly sedated.
What Are the Complications?
The complications of hiatal hernia are:
- Chronic heartburn and inflammation of the lower esophagus, called reflux esophagitis.
- Anemia due to chronic bleeding from the lower esophagus.
- Scarring and narrowing of the lower esophagus causing difficulty in swallowing.
- While sleeping, stomach secretions can seep up the esophagus and into the lungs causing chronic cough, wheezing, and even pneumonia. In addition, the complicated hernia can cause serious problems such as difficulty in breathing or severe chest pain, especially in the elderly.
Treatment
Treatment is called for only when the hernia results in symptoms, such as persistent heartburn or difficulty in swallowing. Acid inflammation and ulceration of the lower esophagus also require treatment. General guidelines for treating heartburn and esophagitis (inflammation of the esophagus) are:
- Avoid (or use only in moderation) foods and substances that increase reflux of acid into the esophagus, such as: nicotine (cigarettes), chocolate, fatty foods, peppermint, alcohol, spearmint, and caffeine.
- Eat smaller, more frequent meals and do not eat within 2-3 hours of bedtime.
- Avoid bending, stooping, abdominal exercises, tight belts, and girdles all of which increase abdominal pressure and cause reflux.
- If overweight, lose weight. Obesity also increases abdominal pressure.
- Prescription medications. Certain drugs, such as intestinal antispasmodics, calcium channel blockers, and some antidepressants weaken the muscle strength of the lower esophagus. Elevate the head of the bed 8 to 10 inches by putting pillows or a wedge under the upper part of the mattress. Gravity then helps keep stomach acid out of the esophagus while sleeping.
Other Treatments
- Drugs - Some medicines effectively reduce the secretion of stomach acid, while others increase the muscle strength of the lower esophagus, thereby reducing acid reflux.
- Surgery - The complicated hiatal hernia requires surgery occasionally on an emergency basis. Surgery otherwise is reserved for those patients with complications that cannot be handled with medications. The mere presence of a hiatal hernia is not a reason for surgery.
Summary
A hiatal hernia is an extremely common condition which usually does not cause symptoms or problems. However, when it does, the physician can frequently treat the problem effectively with a well-planned program. Surgery is infrequently required to treat a hiatal hernia.








