What is Esophageal Dialation?
 The esophagus is the long, narrow food pipe (gullet) that carries food and liquid from the mouth to the stomach. It can become blocked or injured in a variety of ways. Esophageal dilatation is the technique used to stretch or open the blocked portion of the esophagus.
The esophagus is the long, narrow food pipe (gullet) that carries food and liquid from the mouth to the stomach. It can become blocked or injured in a variety of ways. Esophageal dilatation is the technique used to stretch or open the blocked portion of the esophagus.
Causes of Esophageal Blockage
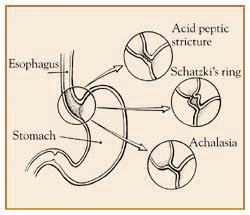
There are several causes of blockage or stricture of the esophagus. They all can make swallowing food and/or fluids difficult. The physician's first job is to find the reason for the stricture or narrowing. The answer can usually be provided by the medical history, physical exam, xrays, and endoscopy (a visual exam of the esophagus using a flexible fiberoptic tube).
- Acid Peptic Stricture - This condition is the most common of all. The stomach produces acid which, in turn, can reflux into the esophagus. This event is frequently worsened by the presence of a hiatus hernia. Over time, the acid and peptic stomach juices injure the esophagus, causing inflammation and then scarring. The fibrous scar then contracts and narrows the esophageal opening.
- Schatzki's Ring - This condition is really exactly that, a narrow ring of benign fibrous tissue constricting the lower esophagus. Physicians still do not know how it develops.
- Ingestion of Caustic Agents - Children are particularly prone to swallowing liquid lye and other agents which can severely burn the esophagus, leaving it narrowed.
- Achalasia - This condition is uncommon and quite fascinating to physicians. The problem is a persistent and marked spasm of the lower esophageal muscle. This spasm just does not open up to allow food and fluid through. The result is a persistent blockage with subsequent slow trickling of the esophageal contents into the stomach.
- Tumors - Various forms of tumors, benign and malignant, can block the esophagus. This condition is obviously very important to diagnose and treat promptly.
- Heredity - The esophagus may be partially or completely blocked at birth.
- Eosinophilic Esophagitis - This is a relatively common narowing of the esophagus usually seen in young individuals.
Methods of Esophageal Dilatation
In most instances, the problem is a mechanical one with an obstruction acting like a dam across a stream. Therefore, the treatment must be mechanical. The dam must be broken. After a diagnosis is made, the physician determines the method of treatment that is in the patient's best interest. The physician has a variety of techniques available. Each has benefits and is appropriate in specific cases. The physician will always discuss these options with the patient.
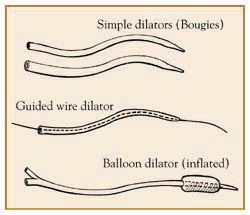
- Simple Dilators (Bougies) - These are a series of flexible dilators of increasing thickness. One or more of these are passed down through the esophagus at a setting. The bougie is the simplest and quickest method of opening the esophagus.
- Guided Wire Bougie - In some instances, the physician performs endoscopy and places a flexible wire across the stricture. The scope is removed and the wire left in place. A dilator with a hole through it from end to end is guided down the esophagus and across the stricture. One or more of these dilators are passed over the wire. At the end of the exam, the wire is removed. This type of treatment may be performed in the x-ray department under fluoroscopy.
- Balloon Dilators - Flexible endoscopy allows the physician to directly view the stricture. Deflated balloons are placed through the scope and across the stricture. When inflated, they become sausage shaped, stretch, and break the stricture.
- Achalasia Dilators - Achalasia is a special situation which requires a larger, balloon-type dilator. The procedure is always done under x-ray control. In this situation, the spastic muscle fibers in the lower esophagus are stretched and broken, which in turn allows easier passage of food and liquid into the stomach.
The Procedure
As mentioned, there are a number, of dilating techniques available to the physician. If endoscopy isperformed at the same time, then it will be done in the endoscopy suite, usually under sedation. X-ray fluoroscopy equipment may be needed, so the procedure is also performed in the x-ray unit. Simple bougie dilatation may take only a few minutes. The other techniques require 20 to 30 minutes. Recovery is usually quick and the patient can soon begin eating and drinking to test the effectiveness of the treatment.
Complications
Esophageal dilatation is usually performed effectively and without problems. However, some complications can occur. A small amount of bleeding almost always happens at the treatment site. At times, it can be excessive, requiring evaluation and treatment. An uncommon but known complication is perforation of the esophagus. The wall of the esophagus is thin and, despite the best efforts of the physician, can tear. An operation may be required to correct this problem.
Alternative Treatments
The alternative treatment options are to do nothing or to undergo major chest surgery. The latter is recommended only if dilatation is ineffective.
In Summary
Narrowing or stricture of the esophagus is a very common problem. The physician can almost always uncover the specific cause of the stricture. There are a variety of treatment options available for the physician. Complications are rare and, in most instances, a satisfactory outcome occurs with complete clearing of or improvement in the swallowing problem.
What is a Colonoscopy?
 |
|
Click and watch this video to get informed about the procedure and it's benefits. |
The term "colonoscopy" means looking inside the colon. It is a procedure performed by a gastroenterologist, a well-trained subspecialist.
The colon, or large bowel, is the last portion of your digestive or GI tract. It starts at the cecum, which attaches to the end of the small intestine, and it ends at the rectum and anus. The colon is a hollow tube, about five feet long, and its main function is to store unabsorbed food products prior to their elimination.
The main instrument that is used to look inside the colon is the colonoscope, which is a long, thin, flexible tube with a tiny video camera and a light on the end. By adjusting the various controls on the colonoscope, the gastroenterologist can carefully guide the instrument in any direction to look at the inside of the colon. The high quality picture from the colonoscope is shown on a TV monitor, and gives a clear, detailed view.
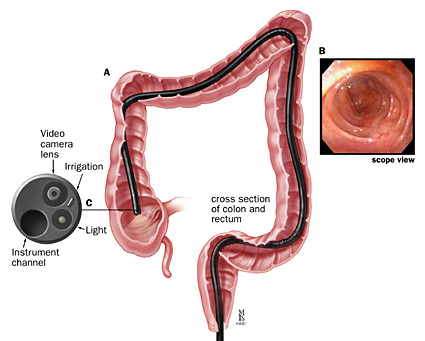
Colonoscopy is more precise than an X-ray. This procedure also allows other instruments to be passed through the colonoscope. These may be used, for example, to painlessly remove a polyp or a suspicious-looking growth or to
take a biopsy, a small piece, for further analysis. In this way, colonoscopy may help to avoid surgery or to better define what type of surgery may need to be done.
Colonoscopy is a safe and effective way to evaluate problems such as blood loss, pain, and changes in bowel habits such as chronic diarrhea or abnormalities that may have first been detected by other tests. Colonoscopy can also identify and treat active bleeding from the bowel.
Colonoscopy is the most accurate test to screen for colorectal cancer, but there is approximately an 8% chance that colorectal cancer will be missed during a colonscopy.
Colonoscopy is also an important way to check for colon cancer and to treat colon polyps, abnormal growths on the inside lining of the intestine. Polyps vary in size and shape and, while most are not cancerous, some may turn into cancer. However, it is not possible to tell just by looking at a polyp if it is malignant or potentially malignant. This is why colonoscopy is often used to remove polyps, a technique called a polypectomy.
How Do I Prepare for a Colonoscopy?
There are important steps that you must take to prepare for the procedure. First, be prepared to give a complete list of all the medicines you are taking, as well as any allergies you have to drugs or other substances. Your medical team will also want to know if you have any other medical conditions that may need special attention before, during, or after the colonoscopy.
You will be given instructions in advance that will outline what you should and should not do in preparation for colonoscopy. Be sure to read and follow these instructions. One very critical step is to thoroughly clean out the colon, which, for many patients, can be the most trying part of the entire exam. It is essential that you complete this step carefully, because how well the bowel is emptied determines the success of the procedure.
Various methods can be used to help cleanse the bowel. Often, a liquid preparation designed to stimulate bowel movements is given by mouth, which may cause bloating. Additional approaches include special diets or the use of enemas. Whatever method or combination of methods that is recommended for you, be sure to follow instructions as directed.
See the "Procedure Preperation" section of the website.
Colonoscopy can be done in either a hospital or outpatient facility. You'll be asked to sign a form that gives your consent to the procedure and states that you understand what is involved. If there is anything you don't understand, ask for more information.
What Can You Expect During a Colonoscopy?
During the procedure, everything will be done to ensure your comfort. An intravenous, or IV, line will be inserted to give you medication to make you relaxed and drowsy. The drug may enable you to remain awake and cooperative, but it may prevent you from remembering much of the experience.
Once you are fully relaxed, your doctor will do a rectal exam with a gloved, lubricated finger; then the lubricated colonoscope will be gently inserted.
As the scope is slowly and carefully passed, you may feel as if you need to move your bowels, and because air is introduced to help advance the scope, you may feel some cramping or fullness. Generally, however, there is little or no discomfort.
The time needed for colonoscopy will vary, but on the average, the procedure takes about 30 minutes. Afterwards, you will be cared for in a recovery area until the effects of the medication have worn off. At this time, your doctor will inform you about the results of your colonoscopy and provide any additional information that you need to know. You'll also be given instructions about how soon you can eat and drink, plus other guidelines for resuming your normal routine.
What are the Possible Complications from a Colonoscopy?
Although colonoscopy is a safe procedure, complications can sometimes occur. These include perforation, a puncture of the colon walls, which could require surgical repair.
When polyp removal or biopsy is performed, hemorrhage (heavy bleeding) may result and sometimes require blood transfusion or reinsertion of the colonoscope to control the bleeding. Be sure to discuss any specific concerns you may have about the procedure with your doctor.
What Can You Expect After Your Colonoscopy?
Occasionally, minor problems may persist, such as bloating, gas, or mild cramping. These symptoms should disappear in 24 hours or less. By the time you're ready to go home, you'll feel stronger and more alert. Nevertheless, rest for the remainder of the day. Have a family member or friend take you home.
A day or so after you're home, you might speak with a member of the colonoscopy team for follow up, or you may have questions you want to ask the doctor directly.
What is Upper GI Endoscopy (EGD)?
The term "endoscopy" refers to a special technique for looking inside a part of the body. "Upper GI" is the portion of the gastrointestinal tract, the digestive system, that includes the esophagus, stomach, duodenum and the beginning of the small intestine. The esophagus carries food from the mouth for digestion in the stomach and duodenum.
Upper GI endoscopy is a procedure performed by a gastroenterologist, a well-trained subspecialist who uses the endoscope to diagnose and, in some cases, treat problems of the upper digestive system.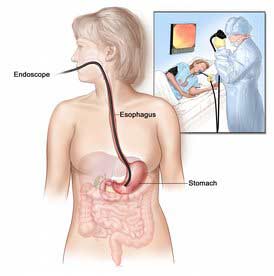
The endoscope is a long, thin, flexible tube with a tiny video camera and light on the end. By adjusting the various controls on the endoscope, the gastroenterologist can safely guide the instrument to carefully examine the inside lining of the upper digestive system. In some cases, it may be necessary to take a sample of tissue, called a biopsy, for later examination under the microscope. This, too, is a painless procedure. In other cases, this endoscope can be used to treat a problem such as active bleeding from an ulcer.
The high quality picture from the endoscope is shown on a TV monitor; it gives a clear, detailed view. In many cases, upper GI endoscopy is a more precise examination than X-ray studies.
Upper GI endoscopy can be helpful in the evaluation or diagnosis of various problems, including difficult or painful swallowing, pain in the stomach or abdomen, and bleeding, indigestion, ulcers, tumors and anemia.
How Do I Prepare for the Procedure?
Regardless of the reason upper GI endoscopy has been recommended for you, there are important steps you can take to prepare for and participate in the procedure. First, be sure to give your doctor a complete list of all the medicines you are taking and any allergies you have to drugs or other substances.
Your medical team will also want to know if you have heart, lung, or other medical conditions that may need special attention before, during, or after upper GI endoscopy. You will be given instructions in advance that will outline what you should and should not do in preparation for the upper GI endoscopy. Be sure to read and follow these instructions.
One very important step in preparing for upper GI endoscopy is that you should not eat or drink within eight to ten hours of your procedure. Food in the stomach will block the view through the endoscope, and it could cause vomiting.
Upper GI endoscopy can be done in either a hospital or outpatient facility. You'll be asked to sign a form that verifies that you consent to having the procedure and that you understand what is involved.
If there is anything you don't understand, ask for more information!
What Can You Expect During an Upper GI Endoscopy?
During the procedure, everything will be done to help you be as comfortable as possible. Your blood pressure, pulse, and the oxygen level in your blood will be carefully monitored. Your doctor will give you a sedative medication; the drug will make you relaxed and drowsy, but you will remain awake enough to cooperate.
You may also have your throat sprayed or be asked to gargle with a local anesthetic to help keep you comfortable as the endoscope is passed. A supportive mouthpiece will be placed to help you keep your mouth open during the endoscopy. Once you are fully prepared, your doctor will gently maneuver the endoscope into position.
As the endoscope is slowly and carefully inserted, air is introduced through it to help your doctor see better. During the procedure, you should feel no pain and it will not interfere with your breathing.
Your doctor will use the endoscope to look closely for any problems that may require evaluation, diagnosis, or treatment.
What are the Possible Complications from an Upper GI Endoscopy?
Years of experience have proved that upper GI endoscopy is a safe procedure. Typically, it takes only 15-20 minutes to perform. Complications rarely occur. These include perforation, a puncture of the esophageal wall, which could require surgical repair, and bleeding, which could require transfusion. Again, these complications are unlikely. Be sure to discuss any specific concerns you may have with your doctor.
When your endoscopy is completed you'll be cared for in a recovery area until most of the effects of the medication have worn off. Your doctor will inform you about the results of the procedure and provide any additional information you need to know.
What Can I Expect After My Upper GI Endoscopy?
You will be given instructions regarding how soon you can eat and drink, plus other guidelines for resuming your normal activity. Occasionally, minor problems may persist, such as mild sore throat, bloating, or cramping; these should disappear in 24 hours or less. By the time you're ready to go home, you'll feel stronger and more alert. Nevertheless, you should plan on resting for the remainder of the day. This means not driving, so you'll need to have a family member or friend take you home. In a few days, you will hear from your doctor with additional information such as results of the biopsy, or you may have questions you want to ask the doctor directly.
What is Flexible Sigmoidoscopy?
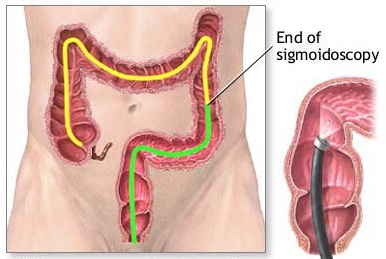
Sigmoidoscopy is the visual examination of the inside of the rectum and sigmoid colon using a lighted, flexible, fiberoptic endoscope. The colon, or large intestine, is 5-6 feet long. During a sigmoidoscopy, only the last 1-2 feet of the colon is examined. This last part of the colon, just above the rectum, is called the sigmoid colon. Equipment
 The flexible endoscope is a remarkable piece of equipment that can be directed and moved around the bends in the lower colon and rectum. A thin, glass fiberoptic bundle collects light in the end of the scope and, regardless of how it is angled, transmits the image to the physician's viewing end. An open channel in the scope allows other instruments to be passed through it to perform biopsies or remove polyps.
The flexible endoscope is a remarkable piece of equipment that can be directed and moved around the bends in the lower colon and rectum. A thin, glass fiberoptic bundle collects light in the end of the scope and, regardless of how it is angled, transmits the image to the physician's viewing end. An open channel in the scope allows other instruments to be passed through it to perform biopsies or remove polyps.
Reasons for the Exam
Sigmoidoscopy is performed because of symptoms or to detect problems at an early stage before they are apparent to the patient.
Bleeding-Rectal bleeding is very common. It often is caused by hemorrhoids or a small tear at the anus, called a fissure. However, more serious problems can cause bleeding. Benign polyps can bleed. It is important to identify and remove polyps at an early stage before they become malignant. Rectal and colon cancer bleed and require immediate diagnosis and treatment. Finally, various forms of colitis and inflammation can cause bleeding.
Diarrhea-Persistent diarrhea should always be evaluated. There are many causes of diarrhea and the exam is of great help in tracking down the specific cause.
Pain-Hemorrhoids and fissures are some causes of pain around the anus or in the rectum. Discomfort in the lower abdomen can be caused by tumors, as well as pockets along the sigmoid colon, called diverticulosis.
X-ray Findings-A barium enema x-ray exam may show abnormalities that need to be confirmed or treated by sigmoidoscopy.
Detection-Colon cancer is one of the most common cancers in the country. It is highly curable if it is found early. This cancer may begin in the colon as a polyp that remains benign for many years. Therefore, it is advisable to have a surveillance exam after a certain age. If there is a history of colon polyps or cancer in parents or siblings, it is even more critical to have this exam because there is a definite hereditary aspect for colon cancer.
Preparation
To obtain the full benefits of the exam, the rectum and sigmoid colon must be clean to allow thorough inspection. Preparation usually involves oral liquids the day before or at supper the night before, along with enemas and/or laxatives. Specific instructions for preparation are always given by the physician's office.
See the "Procedure Preperation" section of the website.
The Procedure
Sigmoidoscopy is performed on an outpatient basis. It is performed with the patient lying on the left side with the right leg drawn up. A sheet is placed over the lower body. A finger or digital exam of the anus and rectum is performed. Then the sigmoidoscope is gently inserted into the rectum. Air is inflated into the bowel to distend it and allow for careful examination. The patient will usually feel this distension of the rectum. The scope is then advanced under direct vision moving around the various bends in the lower bowel.
The scope is advanced as far as possible without causing undue discomfort. When possible, the exam is continued to 60 cm (25 inches). Certain conditions, such as diverticulosis, irritable bowel syndrome or prior pelvic surgery, may produce discomfort when the sigmoid colon is entered. The exam is stopped if this occurs. The entire exam usually takes only 5-10 minutes. Sedation usually is not required.
Benefits
The benefits of sigmoidoscopy are considerable. A specific diagnosis can often be made. A condition, such as colitis, can be monitored following treatment. Polyps and tumors can be discovered at an early stage.
Side Effects and Risks
Bloating and bowel distension are common due to the air inflated into the bowel. This usually lasts only 30-60 minutes. If biopsies are done or if a polyp is removed, there may be some spotting of blood. This is rarely ever serious. One extremely rare risk is a perforation or tear of the sigmoid colon.
In Summary
Sigmoidoscopy is a simple outpatient exam that provides the physician with a great deal of useful information. Specific diagnosis can be made. Treatment programs can be evaluated or reassurance can be provided when the exam is normal. It is one of the most useful and simple exams in medicine. The physician can answer any questions the patient may have.








